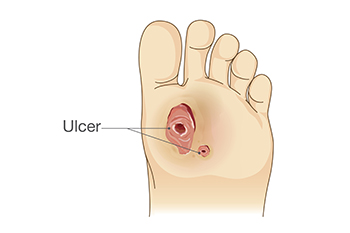
 Chronic foot ulcers are a challenging complication of diabetes. Diabetic ulcers may arise from a variety of factors, including impaired blood circulation, nerve damage, and high blood sugar levels. These factors collectively compromise the body's ability to heal and fight infection. There are many therapies that podiatrists may use to combat foot ulcers, such as advanced wound care techniques, infection control measures, and strategies to enhance circulation. One key treatment is debridement, which involves the careful removal of dead or infected tissue to promote healing. A podiatrist may apply specialized dressings and topical agents that foster a moist healing environment and support tissue regeneration. Another treatment, called offloading, involves reducing pressure on the ulcer through custom footwear or casts. These are not the only treatments that podiatrists may employ. If you are suffering from chronic foot ulcers due to diabetes, it is suggested you schedule regular appointments with a podiatrist to monitor and treat the condition.
Chronic foot ulcers are a challenging complication of diabetes. Diabetic ulcers may arise from a variety of factors, including impaired blood circulation, nerve damage, and high blood sugar levels. These factors collectively compromise the body's ability to heal and fight infection. There are many therapies that podiatrists may use to combat foot ulcers, such as advanced wound care techniques, infection control measures, and strategies to enhance circulation. One key treatment is debridement, which involves the careful removal of dead or infected tissue to promote healing. A podiatrist may apply specialized dressings and topical agents that foster a moist healing environment and support tissue regeneration. Another treatment, called offloading, involves reducing pressure on the ulcer through custom footwear or casts. These are not the only treatments that podiatrists may employ. If you are suffering from chronic foot ulcers due to diabetes, it is suggested you schedule regular appointments with a podiatrist to monitor and treat the condition.
Diabetic foot care is important in preventing foot ailments such as ulcers. If you are suffering from diabetes or have any other concerns about your feet, contact Scott Samera, DPM from Samera / Foot + Ankle. Our doctor can provide the care you need to keep you pain-free and on your feet.
Diabetic Foot Care
Diabetes affects millions of people every year. The condition can damage blood vessels in many parts of the body, especially the feet. Because of this, taking care of your feet is essential if you have diabetes, and having a podiatrist help monitor your foot health is highly recommended.
The Importance of Caring for Your Feet
- Routinely inspect your feet for bruises or sores.
- Wear socks that fit your feet comfortably.
- Wear comfortable shoes that provide adequate support.
Patients with diabetes should have their doctor monitor their blood levels, as blood sugar levels play such a huge role in diabetic care. Monitoring these levels on a regular basis is highly advised.
It is always best to inform your healthcare professional of any concerns you may have regarding your feet, especially for diabetic patients. Early treatment and routine foot examinations are keys to maintaining proper health, especially because severe complications can arise if proper treatment is not applied.
If you have any questions please feel free to contact our office located in Lake City and Branford, FL . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.